Surgical Sterilization Tech Precise Procedures

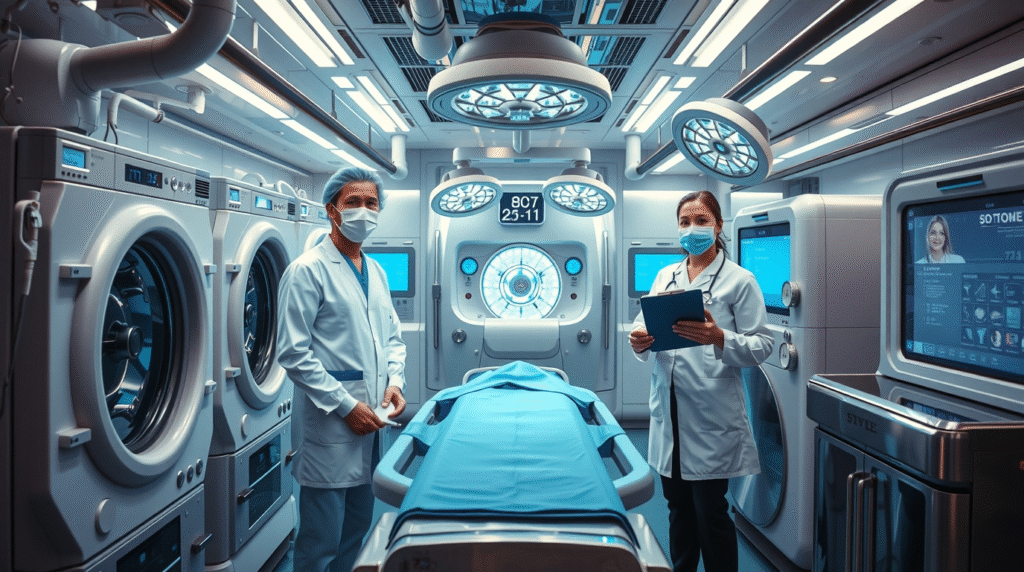
Modern healthcare is evolving faster than ever, and Surgical Sterilization Tech stands at the heart of this transformation. From automated disinfection systems to AI-powered monitoring tools, new technologies are ensuring surgical environments remain completely sterile, safe, and efficient. These innovations not only protect patients but also boost surgical precision and hospital efficiency.
Sterilization technology is not just about cleaning equipment anymore. It’s about building smarter, faster, and more reliable systems that minimize risks and enhance performance. With automation, robotics, and advanced analytics, today’s medical teams can achieve levels of hygiene that were once impossible.

What Is Surgical Sterilization Tech?
Surgical sterilization tech refers to advanced tools and systems designed to remove or destroy all forms of microorganisms from surgical instruments, rooms, and equipment. This includes bacteria, viruses, and spores that may cause infections.
Modern systems use methods like steam sterilization, plasma technology, UV light, and hydrogen peroxide vapor. These techniques are faster, safer, and more effective than traditional manual cleaning. As a result, hospitals can handle more patients while maintaining top hygiene standards.
Why Surgical Sterilization Matters in Modern Medicine
Every surgical procedure carries a risk of infection. Therefore, maintaining a sterile environment is essential. With new sterilization technology, hospitals can minimize contamination and improve patient recovery rates.
These systems also reduce manual labor, allowing medical teams to focus on critical care. Moreover, digital monitoring ensures that every sterilization cycle is validated, recorded, and optimized for safety. Consequently, patient trust increases, and hospital performance improves.
Key Components of Advanced Sterilization Systems
Modern surgical sterilization tech combines various advanced features. Each component works together to ensure full disinfection and reliability. Some major parts include:
- Automated Washers: These systems clean instruments with high-pressure water and detergents.
- Sterilizers (Autoclaves): They use high-temperature steam or gas for complete sterilization.
- Plasma Systems: They employ low-temperature hydrogen peroxide plasma for delicate instruments.
- UV Sterilizers: These use ultraviolet light to destroy bacteria and viruses instantly.
When integrated, these components create a powerful system that supports smooth hospital operations and protects lives.
Role of AI and Automation in Sterilization
AI and automation have transformed surgical sterilization tech into intelligent systems. They can detect performance issues, adjust sterilization cycles, and alert staff if contamination risks arise.
Automated systems reduce human error and ensure consistent hygiene levels. Additionally, AI algorithms analyze data from sterilization equipment to predict maintenance needs and improve operational efficiency. As a result, hospitals save time, reduce costs, and maintain better compliance with safety standards.

Smart Tracking and Real-Time Monitoring
Hospitals now use real-time monitoring to ensure surgical instruments are properly sterilized. Digital systems record every step of the cleaning and sterilization process. This ensures traceability, accountability, and compliance.
RFID tags and barcode systems track instruments through each sterilization phase. Furthermore, smart dashboards alert staff if a cycle fails or if an item needs reprocessing. This continuous monitoring guarantees a sterile surgical environment at all times.
Eco-Friendly Innovations in Sterilization Tech
Environmental safety is becoming a top priority in healthcare. New surgical sterilization tech focuses on using less water, energy, and chemicals. Systems designed with eco-friendly features reduce hospital waste and lower operational costs.
Hydrogen peroxide vapor sterilizers, for example, emit no harmful residues. UV-based systems consume minimal energy while delivering high sterilization performance. By adopting such solutions, healthcare facilities contribute to a sustainable future.
Challenges in Implementing Advanced Sterilization Systems
Although the benefits are clear, hospitals still face challenges when adopting modern surgical sterilization tech. High installation costs, technical training, and equipment compatibility can slow adoption.
However, as healthcare budgets evolve, many organizations recognize the long-term savings of these systems. Improved efficiency, fewer infections, and better compliance make the investment worthwhile. With proper planning and training, the transition becomes smooth and rewarding.
Training and Workforce Readiness
For successful implementation, healthcare staff must understand how new sterilization systems operate. Training programs help them manage digital dashboards, analyze sterilization reports, and maintain equipment performance.
Continuous education keeps teams updated about safety standards and technological upgrades. As automation increases, human oversight remains essential to ensure consistent performance and quality control.
Future Trends in Surgical Sterilization Tech
The future of surgical sterilization tech looks highly innovative. AI integration, IoT sensors, and data analytics will redefine how sterilization is managed. Soon, hospitals will use predictive analytics to schedule cleaning before issues occur.
Wireless sensors will provide live updates on sterilization status. In addition, cloud-based platforms will connect multiple sterilization units, enabling better collaboration between departments and faster decision-making.
Choosing the Right Sterilization Technology
Selecting the best surgical sterilization tech depends on hospital size, budget, and instrument types. Large hospitals may need centralized systems, while smaller clinics benefit from compact sterilizers.
Before investing, facilities should evaluate reliability, safety certifications, and automation compatibility. Proper evaluation ensures that the system meets hygiene standards and supports long-term goals effectively.
Impact of Sterilization Tech on Patient Safety
Ultimately, the purpose of advanced sterilization systems is patient safety. Sterile instruments mean lower infection risks and better recovery outcomes. When hospitals maintain clean surgical environments, they gain patient confidence and medical credibility.
Thus, surgical sterilization tech plays a crucial role in building a safer healthcare ecosystem. As innovation continues, these systems will become smarter, faster, and more sustainable.
Conclusion:
In conclusion, surgical sterilization tech is the backbone of modern healthcare safety. Through automation, AI integration, and smart monitoring, hospitals achieve unmatched hygiene standards. Investing in these technologies ensures cleaner surgeries, safer patients, and stronger medical reputations.
Take action now. Hospitals, clinics, and healthcare leaders should prioritize upgrading to advanced sterilization systems. A sterile environment today means a safer, healthier tomorrow.
FAQs
Q1. What is surgical sterilization tech used for?
It’s used to eliminate all microorganisms from surgical instruments and environments, ensuring patient safety during medical procedures.
Q2. How does AI improve sterilization technology?
AI optimizes sterilization cycles, predicts maintenance needs, and reduces human errors by analyzing real-time performance data.
Q3. Are modern sterilization systems eco-friendly?
Yes, new systems use less water, energy, and chemicals, making them safer for the environment and more cost-efficient.
Q4. What are the main types of sterilization methods?
Common methods include steam sterilization, hydrogen peroxide plasma, UV sterilization, and low-temperature gas systems.




